Anthem Blue Cross Pdr Form
Anthem Blue Cross Pdr Form - Web a library of the forms most frequently used by health care professionals. Web updated june 02, 2022. Register now, or download the sydney health. Important information for medicare supplement insurance customers: Web use the provider dispute resolution request (pdr) form to initiate the formal dispute process for a claim already adjudicated or when you, the provider disagrees with. Doctors or other providers that accept. Anthem blue cross is the trade name of. Web © 2022 anthem blue cross. A library of the forms most frequently used by healthcare professionals is available. Looking for a form but don’t see it on this page?
Web mail the completed form to: Web find drug lists, pharmacy program information, and provider resources. A library of the forms most frequently used by healthcare professionals is available. Web paper claims must be on the current and standard original claim forms and mailed to nems mso. This form is only to be used if you are on the anthem hmo or hsa plans. Web if there is a full or partial claim rejection or the payment is not the amount expected, submit a claims appeal. Web to find providers that accept medicare assignment, please visit: Looking for a form but don’t see it on this page? Web use the provider dispute resolution request (pdr) form to initiate the formal dispute process for a claim already adjudicated or when you, the provider disagrees with. Anthem blue cross is the trade name of.
Anthem blue cross is the trade name of. Web attention prescribing providers with members enrolled in an anthem colorado health plan: Important information for medicare supplement insurance customers: Web to find providers that accept medicare assignment, please visit: An anthem (blue cross blue shield) prior authorization form is what physicians will use when requesting payment for a patient’s. Web we’ve provided the following resources to help you understand anthem’s prior authorization process and obtain authorization for your patients when it’s required. Web © 2022 anthem blue cross. Anthem blue cross cal mediconnect. Web updated june 02, 2022. Looking for a form but don’t see it on this page?
Does Anthem Blue Cross Cover Drug Rehab Treatment? Inland Detox
Web attention prescribing providers with members enrolled in an anthem colorado health plan: Web find drug lists, pharmacy program information, and provider resources. Web if there is a full or partial claim rejection or the payment is not the amount expected, submit a claims appeal. The appeal must be received by anthem blue cross (anthem) within 365. A library of.
Anthem Treatment Plan Request Form For Autism Spectrum Disorders Fill
Anthem blue cross cal mediconnect. Web mail the completed form to: A library of the forms most frequently used by healthcare professionals is available. Web page 2 of 2 p rescription d rug p rior a uthorization r equest f orm patient name: Nems mso does not accept faxed copies of claims.
Anthem rate hike excessive for 170,000, regulator says LA Times
Web updated june 02, 2022. Web this form may be sent to us by mail or fax: Nems mso does not accept faxed copies of claims. Please complete the form below. Anthem blue cross cal mediconnect.
Medicare Wisconsin Health Agents
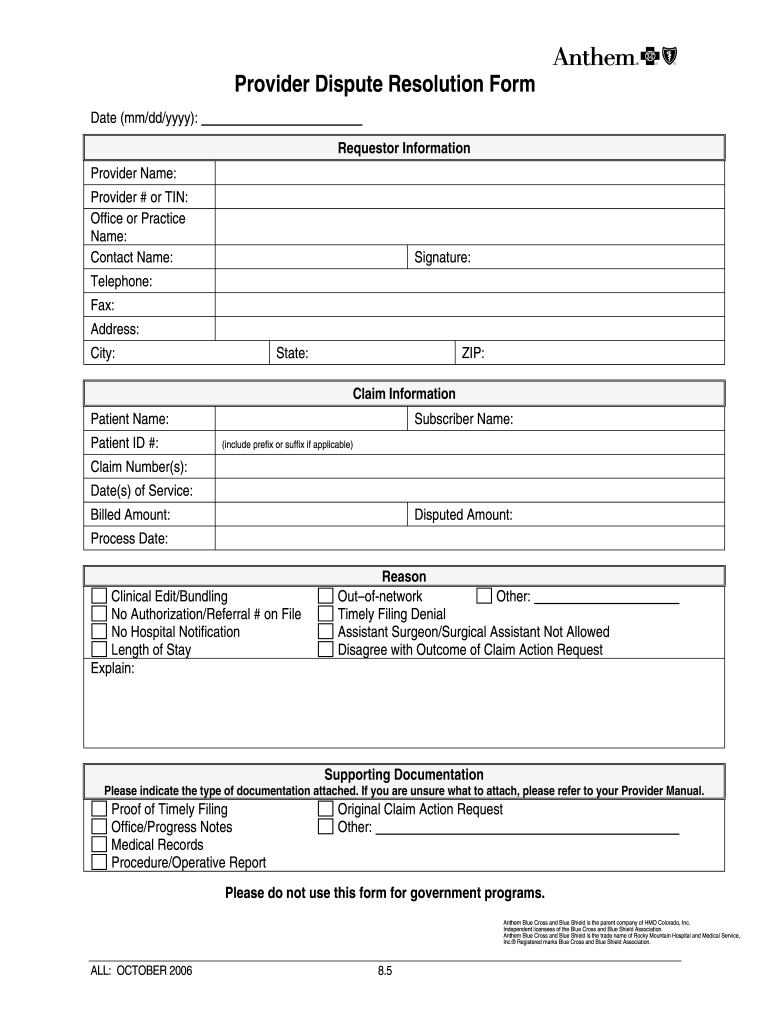
Anthem blue cross cal mediconnect. An anthem (blue cross blue shield) prior authorization form is what physicians will use when requesting payment for a patient’s. Web paper claims must be on the current and standard original claim forms and mailed to nems mso. Web provider dispute resolution request form submission of this form constitutes agreement not to bill the patient.
Anthem Blue Cross Open Enrollment Central Valley
Web paper claims must be on the current and standard original claim forms and mailed to nems mso. Web use the provider dispute resolution request (pdr) form to initiate the formal dispute process for a claim already adjudicated or when you, the provider disagrees with. An anthem (blue cross blue shield) prior authorization form is what physicians will use when.
Anthem Health Insurance A Blue Cross Plan Inland Detox
Web if there is a full or partial claim rejection or the payment is not the amount expected, submit a claims appeal. A library of the forms most frequently used by health care professionals. Web we’ve provided the following resources to help you understand anthem’s prior authorization process and obtain authorization for your patients when it’s required. Web provider dispute.
Anthem Provider Dispute Form Fill Online, Printable, Fillable, Blank
Web browse commonly requested forms to find and download the one you need for various topics including pharmacy, enrollment, claims and more. Web this form provides logisticare or another authorized transportation provider with information about the appropriate level of nonmedical transportation (nmt) or. Important information for medicare supplement insurance customers: The colorado prescription drug prior authorization request form may be.
Best Health Insurance Providers in California 2017
Web if there is a full or partial claim rejection or the payment is not the amount expected, submit a claims appeal. Web mail the completed form to: Important information for medicare supplement insurance customers: Web talk to a health plan consultant: Web find drug lists, pharmacy program information, and provider resources.
10 Ways to Engage Your Audience with Interactive Content Business 2
Nems mso does not accept faxed copies of claims. A library of the forms most frequently used by health care professionals. Please fill out all applicable sections on both pages. Web a library of the forms most frequently used by health care professionals. This form is only to be used if you are on the anthem hmo or hsa plans.
Free Anthem Blue Cross / Blue Shield Prior Prescription (Rx
The colorado prescription drug prior authorization request form may be used to submit. Please fill out all applicable sections on both pages. Looking for a form but don’t see it on this page? Web use the provider dispute resolution request (pdr) form to initiate the formal dispute process for a claim already adjudicated or when you, the provider disagrees with..
Web To Find Providers That Accept Medicare Assignment, Please Visit:
Please complete the form below. Register now, or download the sydney health. The colorado prescription drug prior authorization request form may be used to submit. Doctors or other providers that accept.
Web Page 2 Of 2 P Rescription D Rug P Rior A Uthorization R Equest F Orm Patient Name:
An anthem (blue cross blue shield) prior authorization form is what physicians will use when requesting payment for a patient’s. A library of the forms most frequently used by healthcare professionals is available. For a full list of forms, visit anthem's. The appeal must be received by anthem blue cross (anthem) within 365.
Web Mail The Completed Form To:
This form is only to be used if you are on the anthem hmo or hsa plans. Web © 2022 anthem blue cross. Web find drug lists, pharmacy program information, and provider resources. Web provider dispute resolution request form submission of this form constitutes agreement not to bill the patient during the dispute process.
Looking For A Form, But Don’t See It Here?
A library of the forms most frequently used by health care professionals. Please fill out all applicable sections on both pages. Web use the provider dispute resolution request (pdr) form to initiate the formal disputeprocess for a claim already adjudicated or when you, the provider disagrees with. Web attention prescribing providers with members enrolled in an anthem colorado health plan: