Anthem Blue Cross Provider Dispute Form
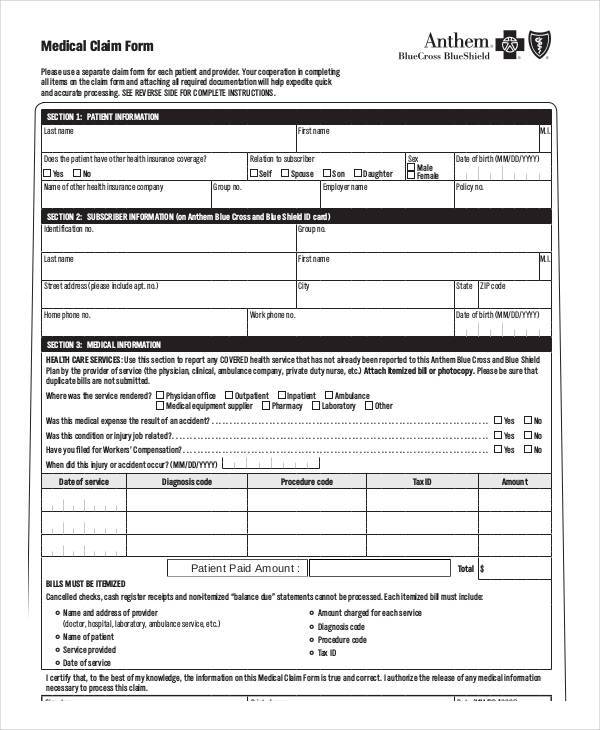
Anthem Blue Cross Provider Dispute Form - Web talk to a health plan consultant: Occurs when a provider disagrees with the medicare advantage (ma) payment; Web up to $40 cash back a healthcare provider or a healthcare professional who is in dispute with a health insurance company or payer would typically be required to file a form for. Web patient name:patient id #: Select dispute the claim to begin the. Involves issues after services have been rendered (handled by calling provider services. Web provider forms & guides. Easily find and download forms, guides, and other related documentation that you need to do business with anthem all in one convenient location! Anthem blue cross and anthem blue cross life and health. Web cross name and symbol are registered marks of the blue cross association.
Anthem blue cross and anthem blue cross life and health. Web lima — ohioans enrolled in anthem blue cross blue shield’s managed medicaid plans are caught in the crosshairs of a dispute between the insurance. Easily fill out pdf blank, edit, and sign them. (including alpha prefix)claim number:date(s) of service:billed amount:process date:explain: Web get answers to your questions about eligibility, benefits, authorizations, claims status and more. Web use the provider maintenance form to submit changes or additions to your information. Easily find and download forms, guides, and other related documentation that you need to do business with anthem all in one convenient location! Complete the appeal request form and send it to: National provider identifier (npi) number:. **any other disputes should be done on the.
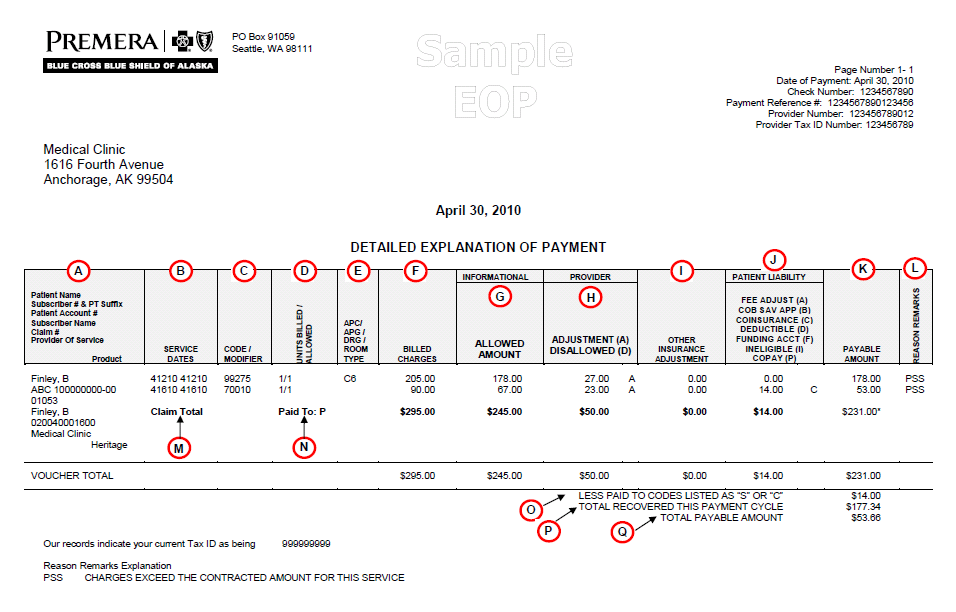
Web cross name and symbol are registered marks of the blue cross association. Web talk to a health plan consultant: Easily fill out pdf blank, edit, and sign them. Web providers (365 days from the eop for out of state providers) • level one claim dispute: Web mail the completed form to: Web provider dispute resolution request form submission of this form constitutes agreement not to bill the patient during the dispute process. Easily find and download forms, guides, and other related documentation that you need to do business with anthem all in one convenient location! National provider identifier (npi) number:. Web use the provider dispute resolution request (pdr) form to initiate the formal dispute process for a claim already adjudicated or when you, the provider. Web up to $40 cash back a healthcare provider or a healthcare professional who is in dispute with a health insurance company or payer would typically be required to file a form for.
Anthem Blue Cross Form For Medical Equipment Reimbursement
If the claim is denied or final, there will be an option to dispute the claim. Claims escalation, disputes, and appeals process. Select a state for information that's relevant to you. If you are unsure which form to complete, please reach out to your provider contract. Save or instantly send your ready documents.
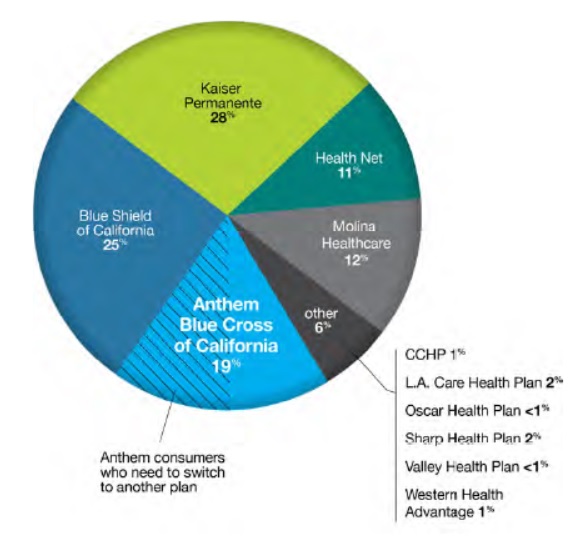
Anthem Blue Cross negotiations with Sutter Health
Select a state for information that's relevant to you. Web mail the completed form to: Web cross name and symbol are registered marks of the blue cross association. Please complete the form below. Easily find and download forms, guides, and other related documentation that you need to do business with anthem all in one convenient location!
Anthem Blue Cross California Grievance Form Blue Cross Blue Shield
Web talk to a health plan consultant: Select a state forms library members can log in to view forms that are specific to their. Please complete the form below. Select a state for information that's relevant to you. Web when submitting a claim payment dispute in writing, providers must include the claim information/ adjustment request 151 form and submit to:
Insurer Anthem Blue Cross, provider resolve dispute on autism therapy
Web georgia provider communications anthem blue cross and blue shield (anthem) provider claims dispute process published: (including alpha prefix)claim number:date(s) of service:billed amount:process date:explain: Web mail the completed form to: Please complete the form below. Web use the provider dispute resolution request (pdr) form to initiate the formal dispute process for a claim already adjudicated or when you, the provider.
Anthem Blue Cross 2018 California Withdrawl cancelling Historical
Save or instantly send your ready documents. Select dispute the claim to begin the. Web talk to a health plan consultant: Claims escalation, disputes, and appeals process. Register now, or download the sydney health.
Does Anthem Blue Cross Cover Drug Rehab Treatment? Inland Detox
Easily fill out pdf blank, edit, and sign them. Web use the provider dispute resolution request (pdr) form to initiate the formal dispute process for a claim already adjudicated or when you, the provider. **any other disputes should be done on the. Web submit an inquiry and review the claims status detail page. Web get answers to your questions about.
Billing Dispute External Review Anthem Blue Cross Doc Template
Web submit an inquiry and review the claims status detail page. Web use the provider maintenance form to submit changes or additions to your information. Register now, or download the sydney health. Providers will not be penalized for filing a claim payment dispute. (including alpha prefix)claim number:date(s) of service:billed amount:process date:explain:
Anthem Blue Cross Provider Forms Video Bokep Ngentot
Register now, or download the sydney health. Web georgia provider communications anthem blue cross and blue shield (anthem) provider claims dispute process published: Please complete the form below. Web provider dispute resolution request form submission of this form constitutes agreement not to bill the patient during the dispute process. Web submit an inquiry and review the claims status detail page.
Anthem provider dispute form Fill out & sign online DocHub
Anthem blue cross and blue shield. Providers will not be penalized for filing a claim payment dispute. **any other disputes should be done on the. Web use the provider maintenance form to submit changes or additions to your information. Web if you disagree with the outcome of a claim, you may begin the anthem blue cross and blue shield (anthem).
BCBS in Provider Dispute Resolution Request Form Blue Cross Blue
(including alpha prefix)claim number:date(s) of service:billed amount:process date:explain: Easily fill out pdf blank, edit, and sign them. Anthem blue cross and blue shield. Providers will not be penalized for filing a claim payment dispute. Web the payment dispute process consists of two internal steps.
Web Use The Provider Dispute Resolution Request (Pdr) Form To Initiate The Formal Dispute Process For A Claim Already Adjudicated Or When You, The Provider.
Web provider dispute resolution request form submission of this form constitutes agreement not to bill the patient during the dispute process. Easily find and download forms, guides, and other related documentation that you need to do business with anthem all in one convenient location! Web blue shield of california healthcare providers can file disputes by printing, filling out, and mailing the appropriate provider dispute resolution form to the right address. If you are unsure which form to complete, please reach out to your provider contract.
Claims Escalation, Disputes, And Appeals Process.
**any other disputes should be done on the. Complete the appeal request form and send it to: Web when submitting a claim payment dispute in writing, providers must include the claim information/ adjustment request 151 form and submit to: Web mail the completed form to:
If The Claim Is Denied Or Final, There Will Be An Option To Dispute The Claim.
Web providers (365 days from the eop for out of state providers) • level one claim dispute: Anthem blue cross and blue shield. Web where do you have or need coverage? Web provider forms & guides.
Easily Fill Out Pdf Blank, Edit, And Sign Them.
Anthem blue cross and anthem blue cross life and health. Web get answers to your questions about eligibility, benefits, authorizations, claims status and more. Occurs when a provider disagrees with the medicare advantage (ma) payment; Involves issues after services have been rendered (handled by calling provider services.