Bcbs Fl Appeal Form
Bcbs Fl Appeal Form - Web mail the form and supporting documentation to: Mail the form and supporting documentation to: Web grievance/appeal form (use this form to initiate a grievance or appeal) (please print or type) please complete all information requested below: Is facing intensifying urgency to stop the worsening fentanyl epidemic. Any other requests will be directed to the appropriate location, which may result in a delay in processing your request. This address is intended for provider um claim appeals only. Web hmo health plan grievance and appeal form for use with myblue, bluecare and simplyblue plans understand that in order for florida blue hmo to review my appeal, they may need medical or other records or information relevant to my appeal. Blue cross and blue shield of florida. Please review the instructions for each category below to ensure proper routing of your appeal. Web the provider clinical appeal form should be used when clinical decision making is necessary:
Web appeals authorizations & referrals claims & billing coordination of patient care pharmacy quality care member forms florida blue members can access a variety of forms including: Web ppo plan appeal form (for use by covered persons with blueoptions and bluechoice group coverage and blueoptions individual coverage) please mail directly to: Web the provider clinical appeal form should be used when clinical decision making is necessary: Medical claims, vision claims and reimbursement forms, prescription drug forms, coverage and premium payment and personal information. Mail the form and supporting documentation to: Web provider appeal form instructions physicians and providers may appeal how a claim processed, paid or denied. Please review the instructions for each category below to ensure proper routing of your appeal. Appeals are divided into two categories: Web hmo health plan grievance and appeal form for use with myblue, bluecare and simplyblue plans understand that in order for florida blue hmo to review my appeal, they may need medical or other records or information relevant to my appeal. Web file a claim health benefits claim form claim appeal form health benefits worldwide vision claim form prescription reimbursement request form mail order prescription form dental claim form travel benefit claim form
Please describe the issue in as much detail as possible. This address is intended for provider um claim appeals only. Web ppo plan appeal form (for use by covered persons with blueoptions and bluechoice group coverage and blueoptions individual coverage) please mail directly to: Web grievance/appeal form (use this form to initiate a grievance or appeal) (please print or type) please complete all information requested below: Drug deaths nationwide hit a record 109,680 in 2022, according to. Web appeals authorizations & referrals claims & billing coordination of patient care pharmacy quality care member forms florida blue members can access a variety of forms including: Web provider appeal form instructions physicians and providers may appeal how a claim processed, paid or denied. Mail the form and supporting documentation to: Web check the applicable box on the provider reconsideration/administrative appeal form. Utilization management adverse determination coding and payment rule please review the instructions for each category below to ensure proper routing of your appeal.
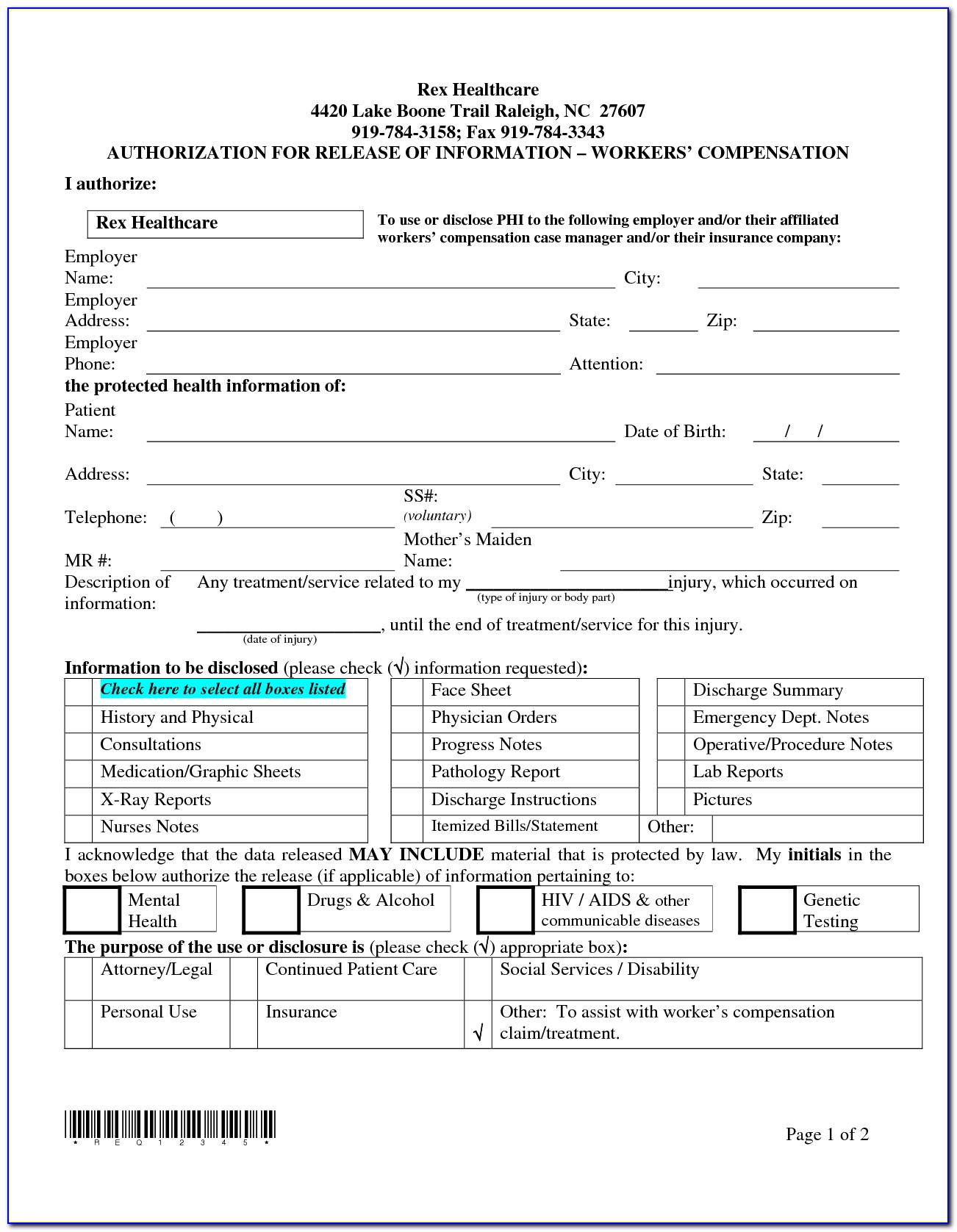
Bcbs Federal Provider Appeal form New Blue Cross Of Mass Giving Opioid
Web file a claim health benefits claim form claim appeal form health benefits worldwide vision claim form prescription reimbursement request form mail order prescription form dental claim form travel benefit claim form Any other requests will be directed to the appropriate location, which may result in a delay in processing your request. Web ppo plan appeal form (for use by.
pare And Contrast The Various Types Governme
This address is intended for provider um claim appeals only. Web file a claim health benefits claim form claim appeal form health benefits worldwide vision claim form prescription reimbursement request form mail order prescription form dental claim form travel benefit claim form Appeals are divided into two categories: Any other requests will be directed to the appropriate location, which may.
BCBS denial code list Medicare denial codes, reason, action and
Mail the form and supporting documentation to: Web check the applicable box on the provider reconsideration/administrative appeal form. Please review the instructions for each category below to ensure proper routing of your appeal. Blue cross and blue shield of florida. Supporting documentation must be submitted.
Bcbs Prior Authorization Form Ohio Form Resume Examples NEpDLPEDxR
Web provider appeal form instructions physicians and providers may appeal how a claim processed, paid or denied. Web the provider clinical appeal form should be used when clinical decision making is necessary: Please review the instructions for each category below to ensure proper routing of your appeal. Mail the form and supporting documentation to: Web the hearing was particularly timely,.
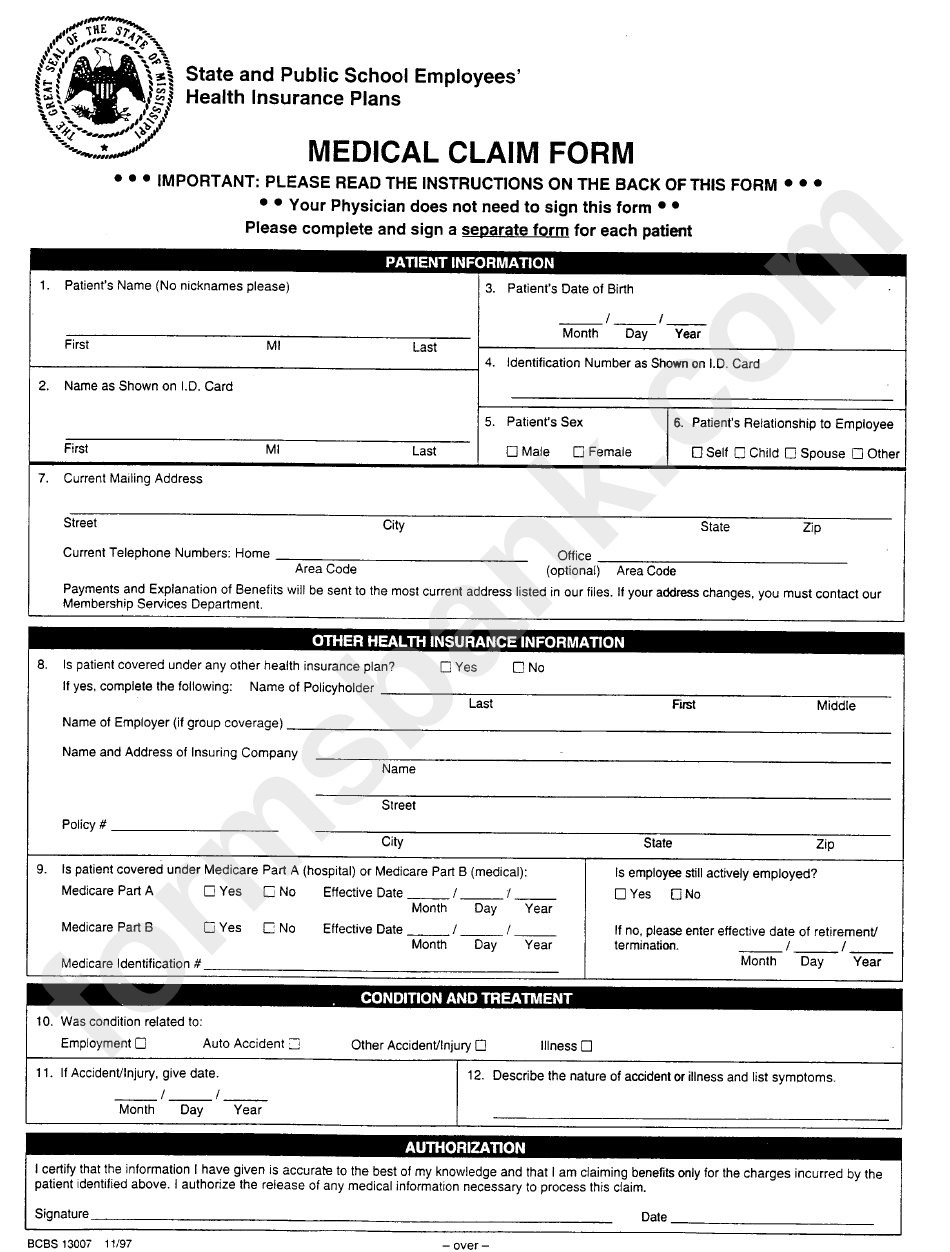
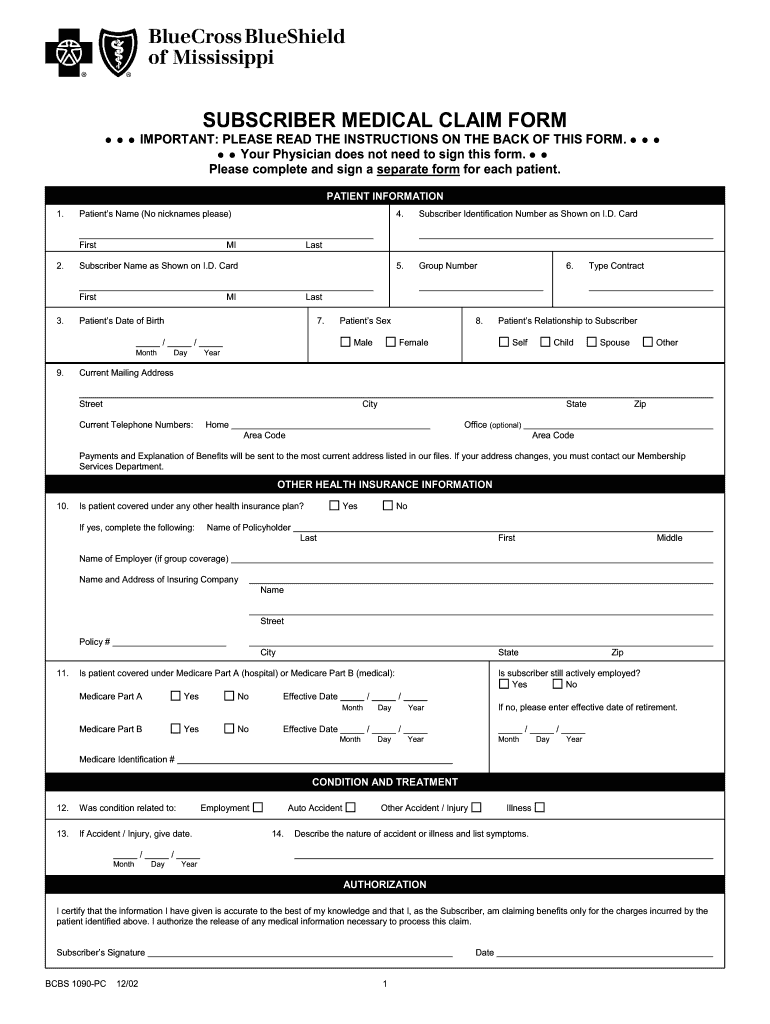
Form Bcbs 13007 State And Public School Employees Medical Claim Form
Please review the instructions for each category below to ensure proper routing of your appeal. Is facing intensifying urgency to stop the worsening fentanyl epidemic. Supporting documentation must be submitted. Utilization management adverse determination coding and payment rule please review the instructions for each category below to ensure proper routing of your appeal. Any other requests will be directed to.
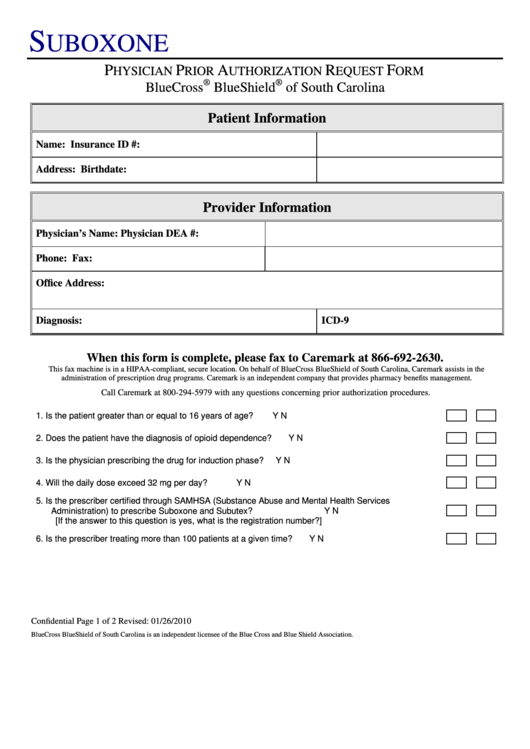
Bcbs Suboxone Physician Prior Authorization Request Form printable pdf
Web hmo health plan grievance and appeal form for use with myblue, bluecare and simplyblue plans understand that in order for florida blue hmo to review my appeal, they may need medical or other records or information relevant to my appeal. Web mail the form and supporting documentation to: Drug deaths nationwide hit a record 109,680 in 2022, according to..
Bcbs Prior Authorization Form Pdf Fill Out and Sign Printable PDF
Web hmo health plan grievance and appeal form for use with myblue, bluecare and simplyblue plans understand that in order for florida blue hmo to review my appeal, they may need medical or other records or information relevant to my appeal. Medical claims, vision claims and reimbursement forms, prescription drug forms, coverage and premium payment and personal information. Web ppo.
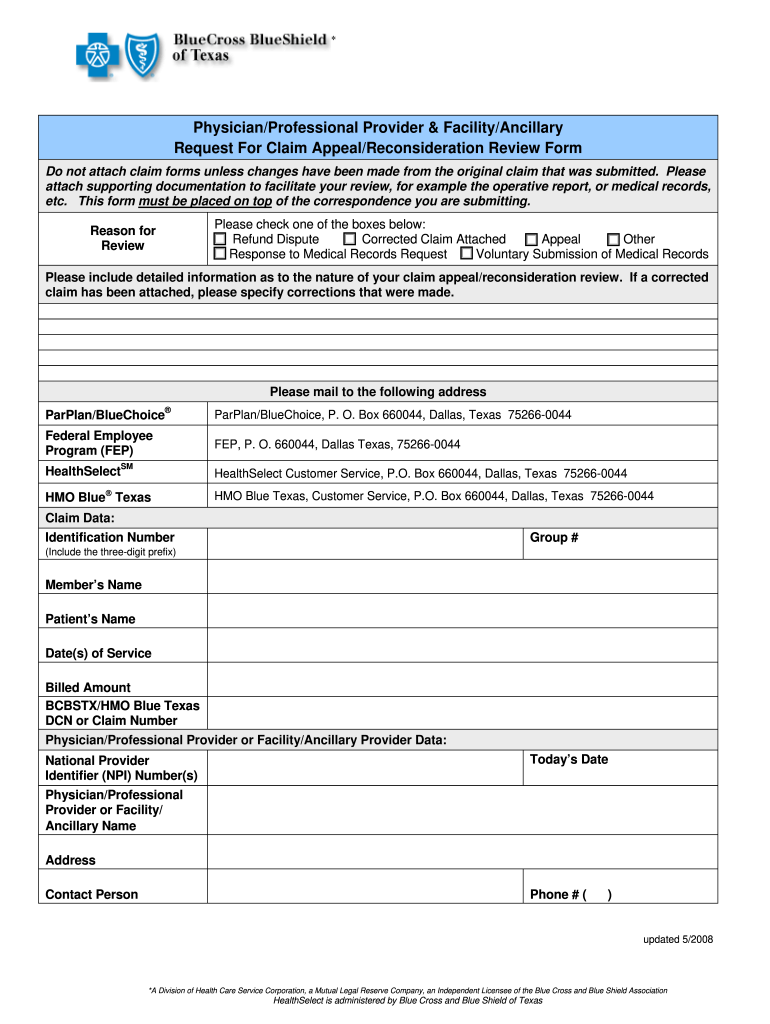
Texas Bcbs Provider Appeal Fill Out and Sign Printable PDF Template
Appeals are divided into two categories: Web mail the form and supporting documentation to: Web hmo health plan grievance and appeal form for use with myblue, bluecare and simplyblue plans understand that in order for florida blue hmo to review my appeal, they may need medical or other records or information relevant to my appeal. Web check the applicable box.
Bcbs fl forms prior auth forms What pharmacy in richmond sales the
Web appeals authorizations & referrals claims & billing coordination of patient care pharmacy quality care member forms florida blue members can access a variety of forms including: Is facing intensifying urgency to stop the worsening fentanyl epidemic. Web the provider clinical appeal form should be used when clinical decision making is necessary: Blue cross and blue shield of florida. This.
Fep Prior Form Bcbs Federal Optumrx Fax Auth Medicare
Web grievance/appeal form (use this form to initiate a grievance or appeal) (please print or type) please complete all information requested below: Web mail the form and supporting documentation to: Mail the form and supporting documentation to: Web appeals authorizations & referrals claims & billing coordination of patient care pharmacy quality care member forms florida blue members can access a.
Web Appeals Authorizations & Referrals Claims & Billing Coordination Of Patient Care Pharmacy Quality Care Member Forms Florida Blue Members Can Access A Variety Of Forms Including:
Appeals are divided into two categories: Web hmo health plan grievance and appeal form for use with myblue, bluecare and simplyblue plans understand that in order for florida blue hmo to review my appeal, they may need medical or other records or information relevant to my appeal. Web grievance/appeal form (use this form to initiate a grievance or appeal) (please print or type) please complete all information requested below: This address is intended for provider um claim appeals only.
Please Review The Instructions For Each Category Below To Ensure Proper Routing Of Your Appeal.
Supporting documentation must be submitted. Drug deaths nationwide hit a record 109,680 in 2022, according to. Blue cross and blue shield of florida. Web check the applicable box on the provider reconsideration/administrative appeal form.
Web File A Claim Health Benefits Claim Form Claim Appeal Form Health Benefits Worldwide Vision Claim Form Prescription Reimbursement Request Form Mail Order Prescription Form Dental Claim Form Travel Benefit Claim Form
Any other requests will be directed to the appropriate location, which may result in a delay in processing your request. Mail the form and supporting documentation to: Medical claims, vision claims and reimbursement forms, prescription drug forms, coverage and premium payment and personal information. Is facing intensifying urgency to stop the worsening fentanyl epidemic.
Web The Hearing Was Particularly Timely, Because The U.s.
Web the provider clinical appeal form should be used when clinical decision making is necessary: Please describe the issue in as much detail as possible. Utilization management adverse determination coding and payment rule please review the instructions for each category below to ensure proper routing of your appeal. Web provider appeal form instructions physicians and providers may appeal how a claim processed, paid or denied.