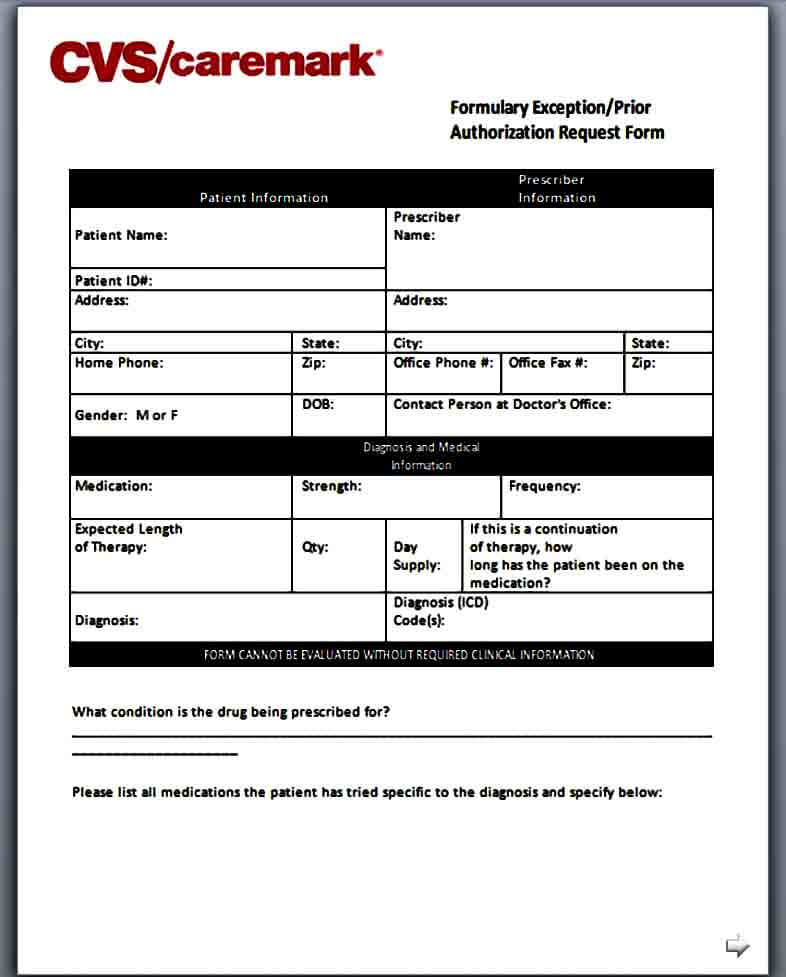
Caremark Prior Auth Form
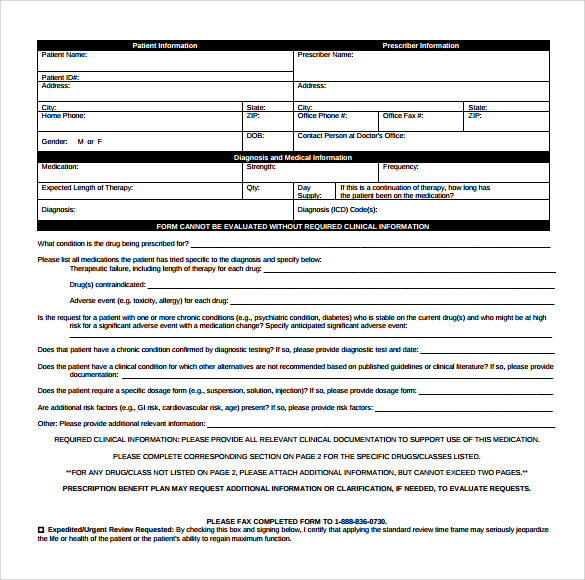
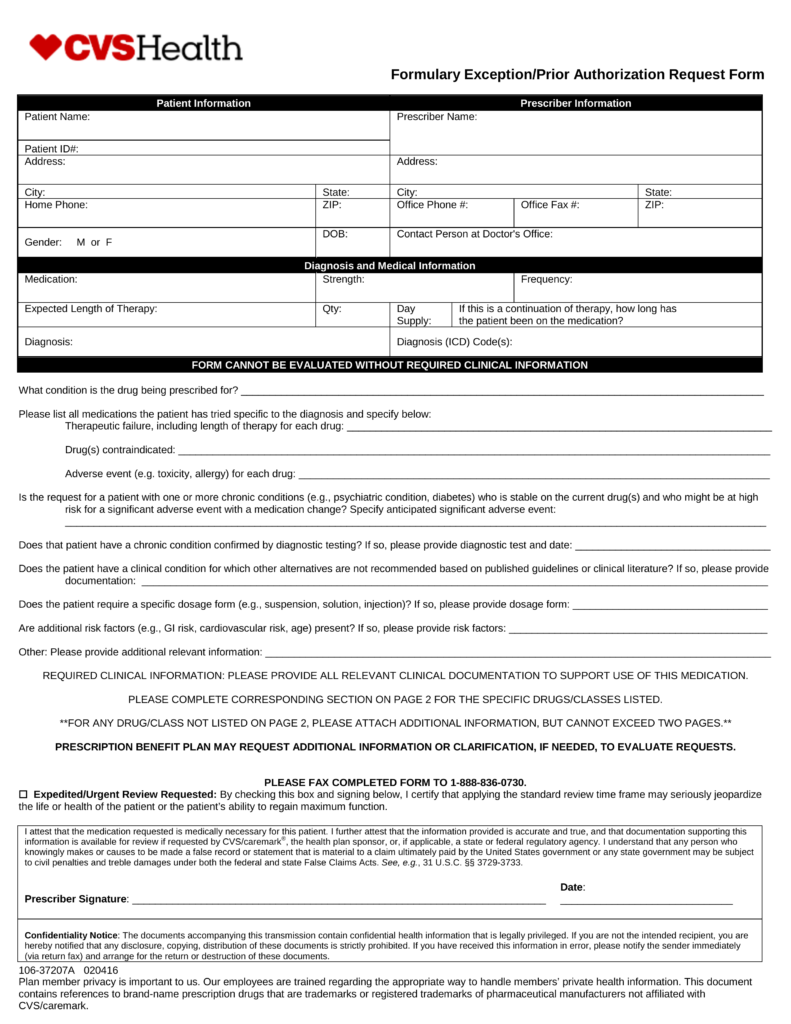
Caremark Prior Auth Form - Covermymeds automates the prior authorization (pa) process making it the fastest and easiest way to review, complete and track pa requests. Web prior authorization forms pa forms for physicians when a pa is needed for a prescription, the member will be asked to have the physician or authorized agent of the physician contact our prior authorization department to answer criteria questions to determine coverage. Cvs caremark reviews this information and, based on your plan, determines whether or not the medication will be covered. By checking this box and signing below, i certify that applying the standard review time frame may seriously jeopardize the life or health of the patient or the patient’s ability to regain maximum function. A physician will need to fill in the form with the patient’s medical information and submit it to cvs/caremark for assessment. Web cvs caremark has made submitting pas easier and more convenient. Use the arrows next to each medication name to expand your selection. Some automated decisions may be communicated in less than 6 seconds! Web formulary exception/prior authorization request form expedited/urgent review requested: Select the starting letter of the name of the medication to begin.
Here is what your colleagues are. A physician will need to fill in the form with the patient’s medical information and submit it to cvs/caremark for assessment. Web formulary exception/prior authorization request form expedited/urgent review requested: Use the arrows next to each medication name to expand your selection. Some automated decisions may be communicated in less than 6 seconds! Covermymeds is cvs caremark prior authorization forms’s preferred method for receiving epa requests. Web prior authorization forms pa forms for physicians when a pa is needed for a prescription, the member will be asked to have the physician or authorized agent of the physician contact our prior authorization department to answer criteria questions to determine coverage. Once we receive your request, we will fax you a drug specific prior authorization request form along with the patient’s specific information and questions that must be answered. Web cvs caremark has made submitting pas easier and more convenient. Web this is called prior authorization, or pa, and it means that your doctor will have to provide additional information on why they are prescribing this medication for you.
Web prior authorization forms pa forms for physicians when a pa is needed for a prescription, the member will be asked to have the physician or authorized agent of the physician contact our prior authorization department to answer criteria questions to determine coverage. Please complete corresponding section for these specific drugs/classes listed below and circle the appropriate. Cvs caremark reviews this information and, based on your plan, determines whether or not the medication will be covered. A physician will need to fill in the form with the patient’s medical information and submit it to cvs/caremark for assessment. Web download, review and print the prior approval form for the requested medication. Once we receive your request, we will fax you a drug specific prior authorization request form along with the patient’s specific information and questions that must be answered. Some automated decisions may be communicated in less than 6 seconds! A cvs/caremark prior authorization form is to be used by a medical office when requesting coverage for a cvs/caremark plan member’s prescription. By checking this box and signing below, i certify that applying the standard review time frame may seriously jeopardize the life or health of the patient or the patient’s ability to regain maximum function. Web formulary exception/prior authorization request form expedited/urgent review requested:
Template Caremark Prior Authorization Form Mous Syusa
Web download, review and print the prior approval form for the requested medication. Cvs caremark reviews this information and, based on your plan, determines whether or not the medication will be covered. Web formulary exception/prior authorization request form patient information prescriber information patient name: Please complete corresponding section for these specific drugs/classes listed below and circle the appropriate. A physician.
CVS Caremark 10637207A 20192021 Fill and Sign Printable Template
A physician will need to fill in the form with the patient’s medical information and submit it to cvs/caremark for assessment. Once we receive your request, we will fax you a drug specific prior authorization request form along with the patient’s specific information and questions that must be answered. Covermymeds is cvs caremark prior authorization forms’s preferred method for receiving.
Template Caremark Prior Authorization Form Mous Syusa
Here is what your colleagues are. Cvs caremark reviews this information and, based on your plan, determines whether or not the medication will be covered. Covermymeds is cvs caremark prior authorization forms’s preferred method for receiving epa requests. A abilify mycite absorica (brand only) abstral aciphex (generic only) actemra acthar gel actimmune actiq aczone adakveo adbry Prior authorization can ensure.
FREE 8+ Sample Caremark Prior Authorization Forms in PDF
By checking this box and signing below, i certify that applying the standard review time frame may seriously jeopardize the life or health of the patient or the patient’s ability to regain maximum function. Web cvs caremark has made submitting pas easier and more convenient. Web select the appropriate cvs caremark form to get started. Web prior authorization forms pa.
Info Caremark Epa Form Fill Out and Sign Printable PDF Template signNow
Web updated june 02, 2022. By checking this box and signing below, i certify that applying the standard review time frame may seriously jeopardize the life or health of the patient or the patient’s ability to regain maximum function. Once we receive your request, we will fax you a drug specific prior authorization request form along with the patient’s specific.
cvscaremarkpriorauthorizationform600x800 Free Job Application Form
Once we receive your request, we will fax you a drug specific prior authorization request form along with the patient’s specific information and questions that must be answered. A physician will need to fill in the form with the patient’s medical information and submit it to cvs/caremark for assessment. Covermymeds is cvs caremark prior authorization forms’s preferred method for receiving.
Free CVS/Caremark Prior (Rx) Authorization Form PDF eForms
Covermymeds automates the prior authorization (pa) process making it the fastest and easiest way to review, complete and track pa requests. Web formulary exception/prior authorization request form expedited/urgent review requested: Web formulary exception/prior authorization request form patient information prescriber information patient name: Web updated june 02, 2022. Once we receive your request, we will fax you a drug specific prior.
FREE 8+ Sample Prior Authorization Forms in PDF MS Word
Web formulary exception/prior authorization request form patient information prescriber information patient name: Please complete corresponding section for these specific drugs/classes listed below and circle the appropriate. Web updated june 02, 2022. Here is what your colleagues are. Cvs caremark reviews this information and, based on your plan, determines whether or not the medication will be covered.
Cvs Caremark Appeal Form Fill Out and Sign Printable PDF Template
Prior authorization can ensure proper patient selection, dosage, drug administration and duration of selected drugs. Here is what your colleagues are. Web updated june 02, 2022. We've partnered with covermymeds ® and surescripts ®, making it easy for you to access electronic prior authorization (epa) via the epa vendor of your choice. Once we receive your request, we will fax.
Cvs Caremark Prior Auth Form Pdf
We've partnered with covermymeds ® and surescripts ®, making it easy for you to access electronic prior authorization (epa) via the epa vendor of your choice. Web updated june 02, 2022. Web this is called prior authorization, or pa, and it means that your doctor will have to provide additional information on why they are prescribing this medication for you..
Web Formulary Exception/Prior Authorization Request Form Expedited/Urgent Review Requested:
By checking this box and signing below, i certify that applying the standard review time frame may seriously jeopardize the life or health of the patient or the patient’s ability to regain maximum function. Web this is called prior authorization, or pa, and it means that your doctor will have to provide additional information on why they are prescribing this medication for you. Select the starting letter of the name of the medication to begin. Some automated decisions may be communicated in less than 6 seconds!
Covermymeds Is Cvs Caremark Prior Authorization Forms’s Preferred Method For Receiving Epa Requests.
A cvs/caremark prior authorization form is to be used by a medical office when requesting coverage for a cvs/caremark plan member’s prescription. Prior authorization can ensure proper patient selection, dosage, drug administration and duration of selected drugs. Please complete corresponding section for these specific drugs/classes listed below and circle the appropriate. Cvs caremark reviews this information and, based on your plan, determines whether or not the medication will be covered.
Cvs Caremark Prior Authorization (Pa) Tools Are Developed To Ensure Safe, Effective And Appropriate Use Of Selected Drugs.
Here is what your colleagues are. Covermymeds automates the prior authorization (pa) process making it the fastest and easiest way to review, complete and track pa requests. Web updated june 02, 2022. Web select the appropriate cvs caremark form to get started.
Web Formulary Exception/Prior Authorization Request Form Patient Information Prescriber Information Patient Name:
Use the arrows next to each medication name to expand your selection. Web prior authorization forms pa forms for physicians when a pa is needed for a prescription, the member will be asked to have the physician or authorized agent of the physician contact our prior authorization department to answer criteria questions to determine coverage. A abilify mycite absorica (brand only) abstral aciphex (generic only) actemra acthar gel actimmune actiq aczone adakveo adbry Once we receive your request, we will fax you a drug specific prior authorization request form along with the patient’s specific information and questions that must be answered.