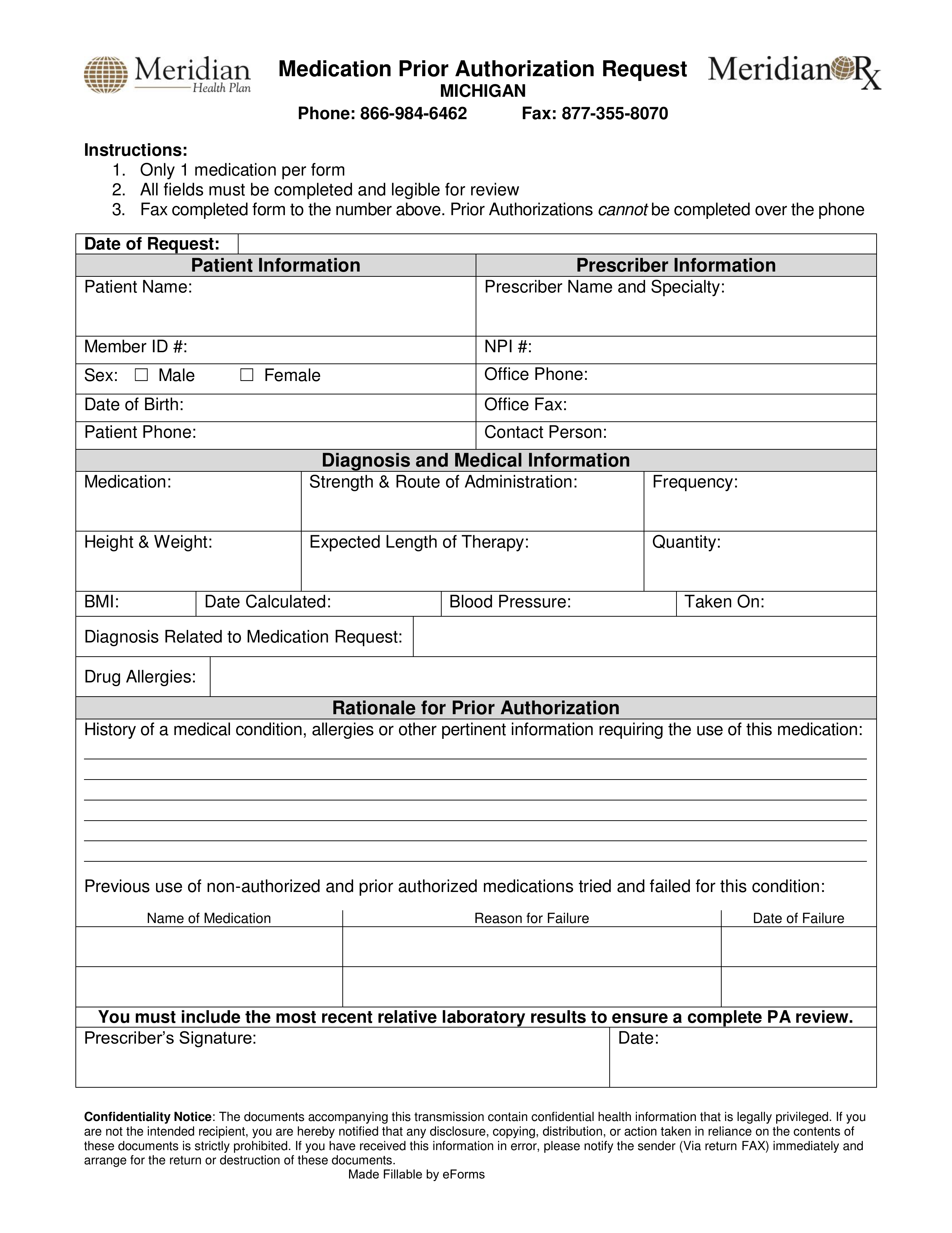
Meridian Authorization Form
Meridian Authorization Form - Edit meridian prior authorization form. Web yes no to submit a prior authorization login here. Web up to $40 cash back prepare a file. All fields must be completed and legible for review. Web once you have created an account, you can use the meridian provider portal to: Then upload your file to the system from your device, importing it from internal mail, the cloud, or by adding its url. Web authorization form complete and fax to: Web the process for access. Ad register and subscribe now to work on meridian medicaid prior authorization overwiew form. Web prior authorization is required before certain services are rendered to confirm medical necessity as defined by the member’s plan.
Web the process for access. Web prior authorization is required before certain services are rendered to confirm medical necessity as defined by the member’s plan. Web authorization form complete and fax to: Web inpatient authorization form (pdf) outpatient authorization form (pdf) clinical policy: Whether submitting exam requests or checking the. Web once you have created an account, you can use the meridian provider portal to: Prior authorizations cannot be submittedover the phone. To submit electronically, go to meridianrx.com and select “submit prior authorization.” Web yes no to submit a prior authorization login here. To request a copy of your medical records, please complete this form.
Web yes no to submit a prior authorization login here. And select “submit prior authorization.” date of request: Web once you have created an account, you can use the meridian provider portal to: Web authorization form complete and fax to: Use the add new button. You do not need a paper referral from meridian to see a provider, but your provider may need to request a prior authorization from meridian for a service to. Web some covered services or medications may need approval from meridian, this is called a prior authorization (pa). Only 1 medication per form all fields must be completed and legible for review. Web the process for access. Prior authorizations cannot be submittedover the phone.
Member Service Area MeridianHealth of Michigan
Only 1 medication per form 2. To submit electronically, go to meridianrx.com and select “submit prior authorization.” (nia) that provides ordering and rendering providers with instant access to prior authorization requests for specialty procedures. All fields must be completed and legible for review. Then upload your file to the system from your device, importing it from internal mail, the cloud,.
Free Meridian Prior (Rx) Authorization Form PDF eForms
Web prior authorization is required before certain services are rendered to confirm medical necessity as defined by the member’s plan. Web inpatient authorization form (pdf) outpatient authorization form (pdf) clinical policy: The authorization form should be signed in the presence of a meridian staff member or signed in the presence of, and witnessed by, another agency or professional office or..
Meridian Gardens Printable Order Form/Wish List, Dorsey, Illinois
Ad register and subscribe now to work on meridian medicaid prior authorization overwiew form. Web yes no to submit a prior authorization login here. This portal is for dates of service on or after 4/1/22. And select “submit prior authorization.” date of request: If an authorization is needed, you can access our login to submit.
Authorized Representative Designation Form Meridian
Web yes no to submit a prior authorization login here. Prior authorizations cannot be submittedover the phone. Rearrange and rotate pages, add and edit text, and use. Web up to $40 cash back prepare a file. Prior authorizations cannot be submitted over the phone.
Meridian Health Plan Medication Prior Authorization Form Illinois
Use the add new button. All fields must be completed and legible for review. Web yes no to submit a prior authorization login here. Web prior authorization is required before certain services are rendered to confirm medical necessity as defined by the member’s plan. Only 1 medication per form all fields must be completed and legible for review.
Request an Estimate Meridian Meridian Automation, Communication
All fields must be completed and legible for review. Only 1 medication per form all fields must be completed and legible for review. Tools and resources specific clinical criteria available within the information linked below: Only 1 medication per form 2. Then upload your file to the system from your device, importing it from internal mail, the cloud, or by.
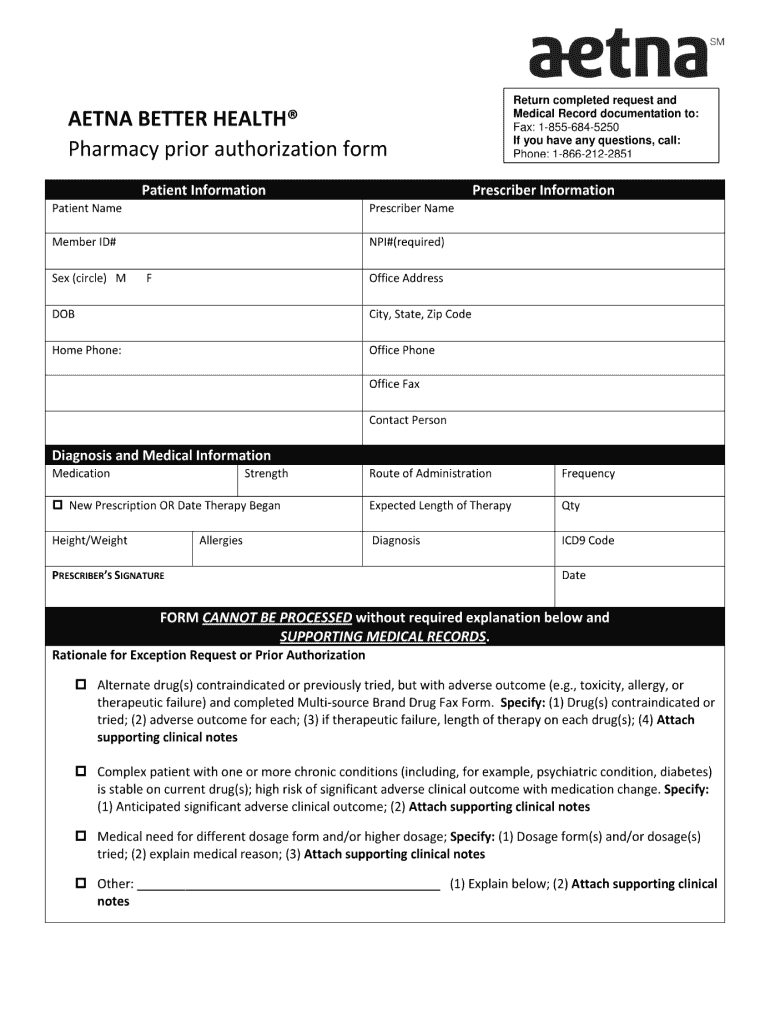
Aetna Prior Authorization Form Pdf Fill Out and Sign Printable PDF
And select “submit prior authorization.” date of request: Then upload your file to the system from your device, importing it from internal mail, the cloud, or by adding its url. Web up to $40 cash back prepare a file. Whether submitting exam requests or checking the. Prior authorizations cannot be submitted over the phone.
2020 Sunshine Health Inpatient Medicaid Prior Authorization Fax Form
And select “submit prior authorization.” date of request: Mobile crisis response provider reference guide. (nia) that provides ordering and rendering providers with instant access to prior authorization requests for specialty procedures. Web up to $40 cash back prepare a file. You do not need a paper referral from meridian to see a provider, but your provider may need to request.
Member Portal Meridian Choice
Prior authorizations cannot be submittedover the phone. Web some covered services or medications may need approval from meridian, this is called a prior authorization (pa). Web prior authorization is required before certain services are rendered to confirm medical necessity as defined by the member’s plan. Tools and resources specific clinical criteria available within the information linked below: Rearrange and rotate.
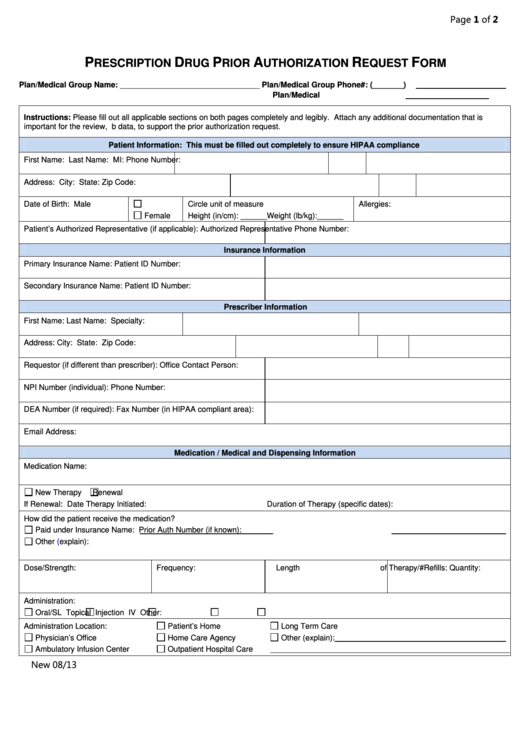
Fillable Prescription Drug Prior Authorization Request Form printable
Rearrange and rotate pages, add and edit text, and use. To submit electronically, go to meridianrx.com and select “submit prior authorization.” This portal is for dates of service on or after 4/1/22. Use the add new button. Tools and resources specific clinical criteria available within the information linked below:
Web Authorization Form Complete And Fax To:
Web prior authorization is required before certain services are rendered to confirm medical necessity as defined by the member’s plan. Web inpatient authorization form (pdf) outpatient authorization form (pdf) clinical policy: Edit meridian prior authorization form. Rearrange and rotate pages, add and edit text, and use.
Web The Process For Access.
(nia) that provides ordering and rendering providers with instant access to prior authorization requests for specialty procedures. And select “submit prior authorization.” date of request: Web some covered services or medications may need approval from meridian, this is called a prior authorization (pa). The authorization form should be signed in the presence of a meridian staff member or signed in the presence of, and witnessed by, another agency or professional office or.
Mobile Crisis Response Provider Reference Guide.
You do not need a paper referral from meridian to see a provider, but your provider may need to request a prior authorization from meridian for a service to. Tools and resources specific clinical criteria available within the information linked below: If an authorization is needed, you can access our login to submit. Only 1 medication per form all fields must be completed and legible for review.
To Request A Copy Of Your Medical Records, Please Complete This Form.
Prior authorizations cannot be submittedover the phone. Only 1 medication per form 2. Then upload your file to the system from your device, importing it from internal mail, the cloud, or by adding its url. Use the add new button.