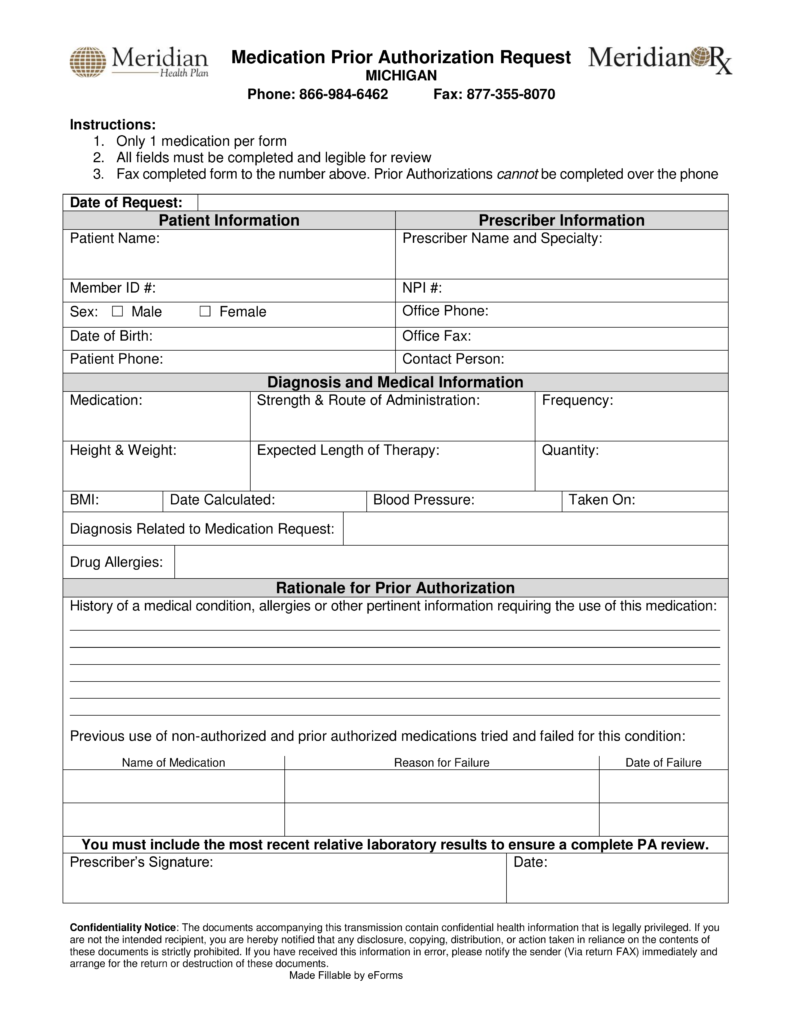
Meridian Prior Auth Form
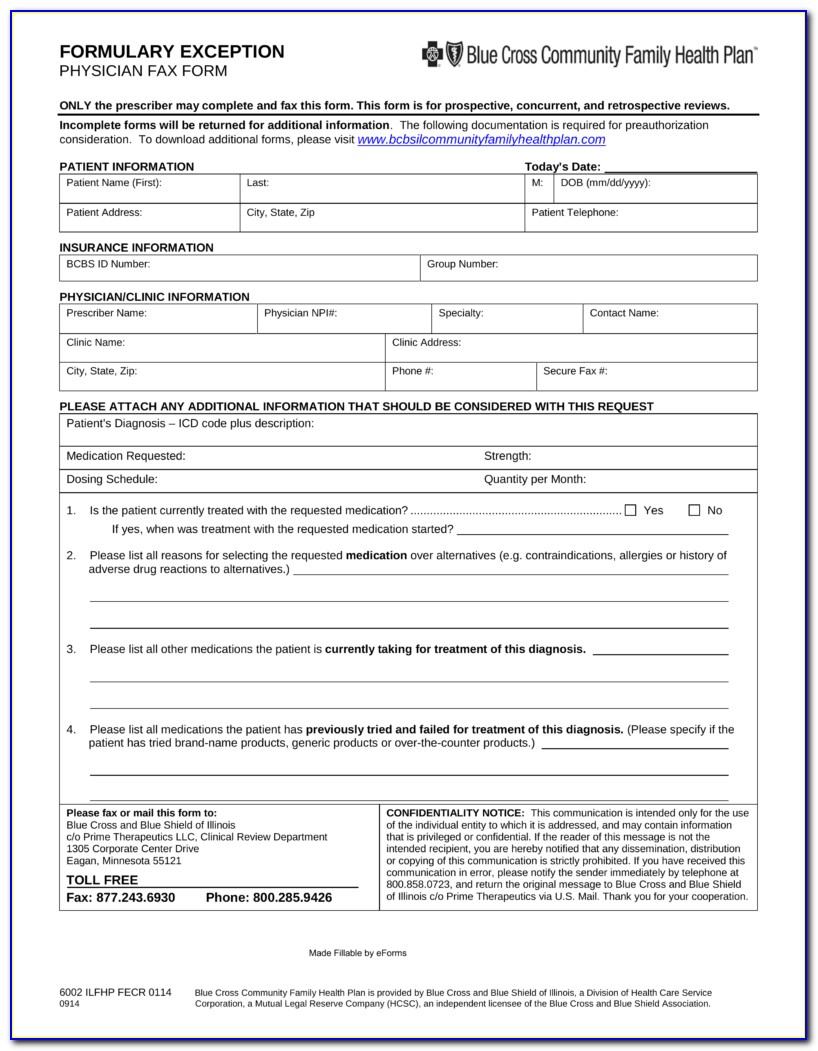
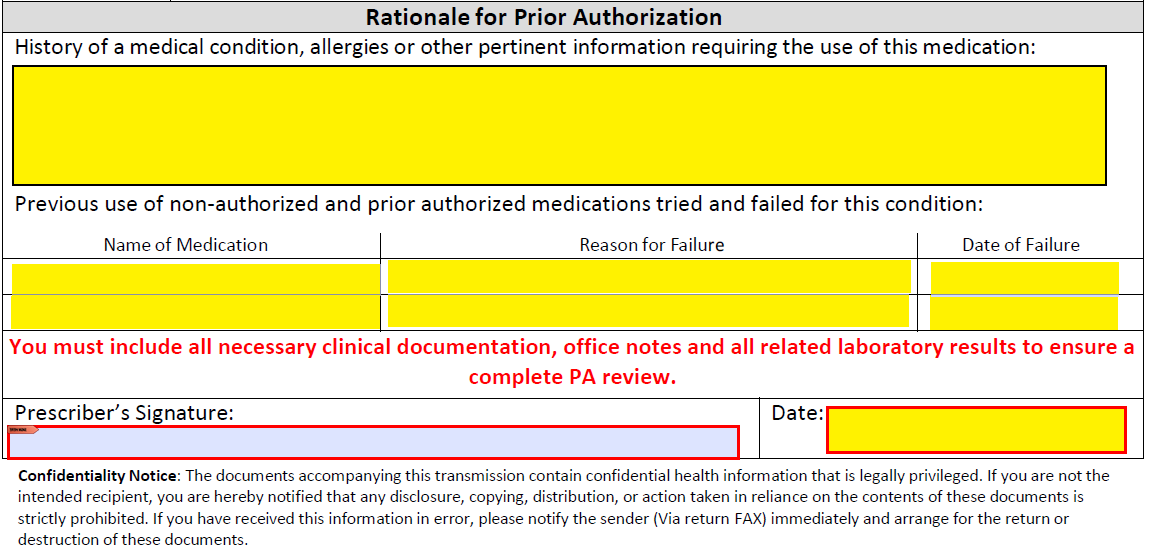
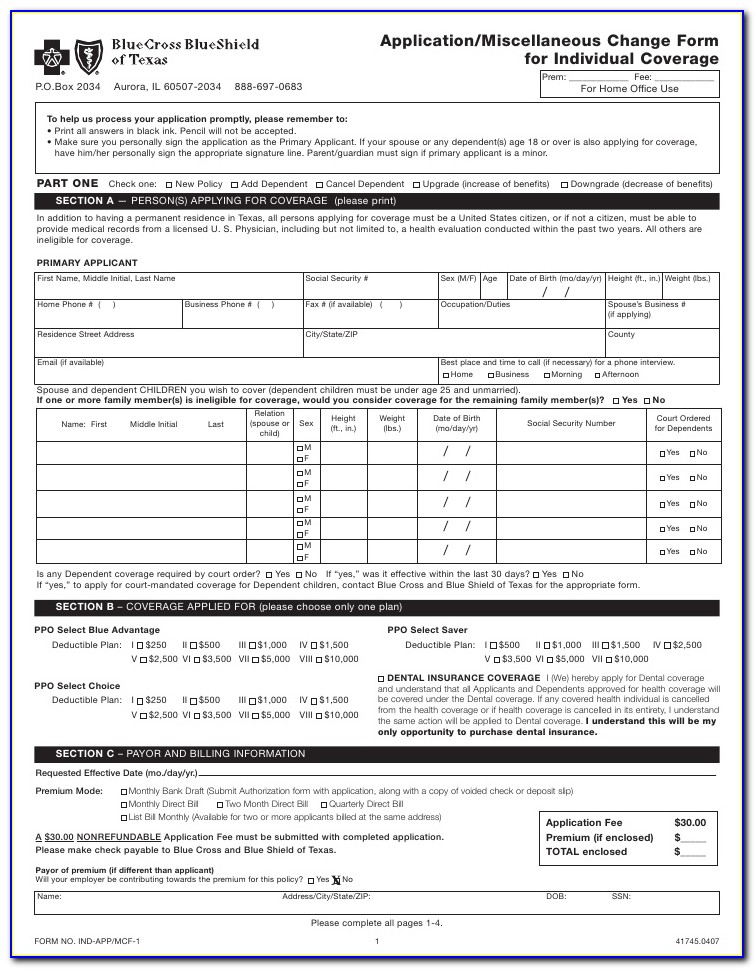
Meridian Prior Auth Form - Only 1 medication per form all fields must be completed and legible for review. Web prior authorization is required before certain services are rendered to confirm medical necessity as defined by the member’s plan. To submit electronically, go to meridianrx.com and select “submit prior authorization.” Weight watchers® exhausted benefit form You do not need a paper referral from meridian to see a provider, but your provider may need to request a prior authorization from. The following information is required for meridian to accept your authorization request: Web meridian prior (rx) authorization form. Mobile crisis response provider reference guide. Web effective april 1, 2022, the electronic prior authorization (epa) form will no longer be an acceptable form of submission. Web some covered services or medications may need approval from meridian, this is called a prior authorization (pa).
Only 1 medication per form all fields must be completed and legible for review. Web prior authorization is required before certain services are rendered to confirm medical necessity as defined by the member’s plan. Please visit our new prior authorization website page to gain access to the secure portal and correct fax forms here. Prior authorizations cannot be submitted over the phone. Web meridian prior (rx) authorization form. Web effective april 1, 2022, the electronic prior authorization (epa) form will no longer be an acceptable form of submission. Primary care provider reassignment form. Web some covered services or medications may need approval from meridian, this is called a prior authorization (pa). You do not need a paper referral from meridian to see a provider, but your provider may need to request a prior authorization from. Prior authorizations should be submitted through the new provider portal or via fax.
Weight watchers® exhausted benefit form A physician may be able to secure insurance coverage and obtain clearance to prescribe the proposed medication once the below form has been. The following information is required for meridian to accept your authorization request: Mobile crisis response provider reference guide. Web meridian prior (rx) authorization form. Web prior authorization is required before certain services are rendered to confirm medical necessity as defined by the member’s plan. Prior authorizations should be submitted through the new provider portal or via fax. Web medication prior authorization request phone: If an authorization is needed, you can access our login to submit online. Primary care provider reassignment form.
Free Meridian Prior (Rx) Authorization Form PDF eForms
Web some covered services or medications may need approval from meridian, this is called a prior authorization (pa). A physician may be able to secure insurance coverage and obtain clearance to prescribe the proposed medication once the below form has been. Prior authorizations cannot be submitted over the phone. Web meridian prior (rx) authorization form. Prior authorizations should be submitted.
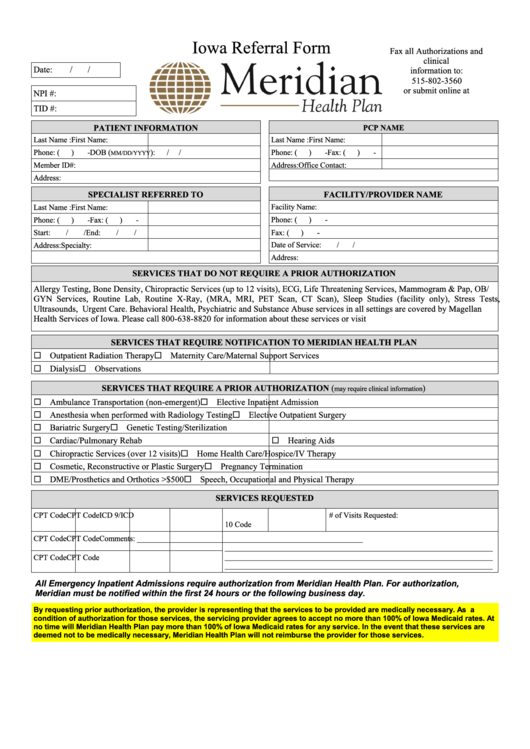
Fillable Iowa Referral Form Meridian Health Plan printable pdf download
• full name of member • member’s date of birth • member’s meridian id number Web meridian prior (rx) authorization form. Primary care provider reassignment form. A physician may be able to secure insurance coverage and obtain clearance to prescribe the proposed medication once the below form has been. Web effective april 1, 2022, the electronic prior authorization (epa) form.
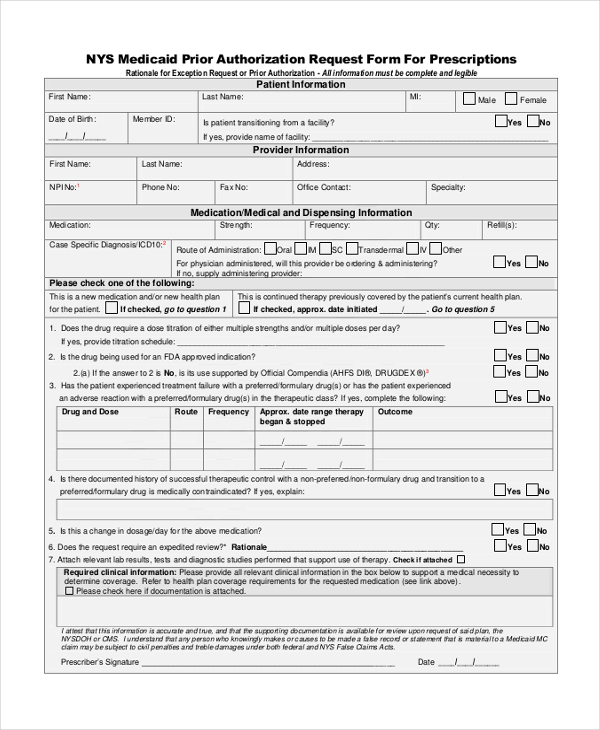
FREE 10+ Sample Medical Authorization Forms in PDF MS Word Excel
Prior authorizations should be submitted through the new provider portal or via fax. Primary care provider reassignment form. Web medication prior authorization request phone: Mobile crisis response provider reference guide. The following information is required for meridian to accept your authorization request:
Contact
Weight watchers® exhausted benefit form Please visit our new prior authorization website page to gain access to the secure portal and correct fax forms here. Web some covered services or medications may need approval from meridian, this is called a prior authorization (pa). Mobile crisis response provider reference guide. Web prior authorization is required before certain services are rendered to.
Michigan Information Meridian
Prior authorizations should be submitted through the new provider portal or via fax. Weight watchers® exhausted benefit form You do not need a paper referral from meridian to see a provider, but your provider may need to request a prior authorization from. The following information is required for meridian to accept your authorization request: A physician may be able to.
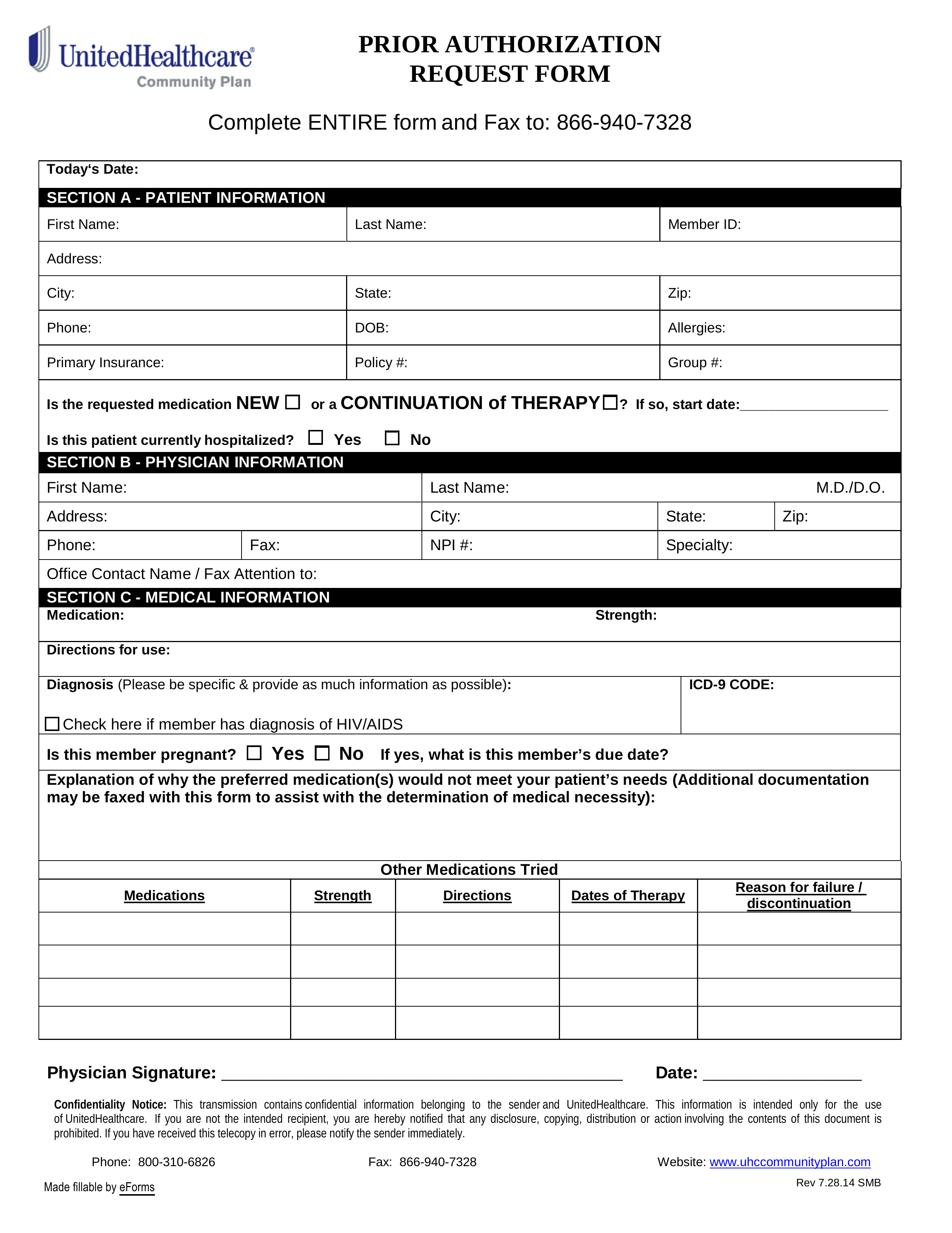
Free UnitedHealthcare Prior (Rx) Authorization Form PDF eForms
Primary care provider reassignment form. Only 1 medication per form all fields must be completed and legible for review. Web meridian prior (rx) authorization form. If an authorization is needed, you can access our login to submit online. You do not need a paper referral from meridian to see a provider, but your provider may need to request a prior.
Covermymeds Humana Prior Auth Form Form Resume Examples bX5aVMLOwW
If an authorization is needed, you can access our login to submit online. Primary care provider reassignment form. Web medication prior authorization request phone: Weight watchers® exhausted benefit form • full name of member • member’s date of birth • member’s meridian id number
Free Meridian Prior Prescription (Rx) Authorization Form PDF
You do not need a paper referral from meridian to see a provider, but your provider may need to request a prior authorization from. • full name of member • member’s date of birth • member’s meridian id number Only 1 medication per form all fields must be completed and legible for review. A physician may be able to secure.
Meridian Health Plan Medication Prior Authorization Form Illinois
Only 1 medication per form all fields must be completed and legible for review. Web prior authorization is required before certain services are rendered to confirm medical necessity as defined by the member’s plan. Web welcome michigan complete members. A physician may be able to secure insurance coverage and obtain clearance to prescribe the proposed medication once the below form.
Covermymeds Humana Prior Auth Form Form Resume Examples bX5aVMLOwW
Only 1 medication per form all fields must be completed and legible for review. Primary care provider reassignment form. Web some covered services or medications may need approval from meridian, this is called a prior authorization (pa). You do not need a paper referral from meridian to see a provider, but your provider may need to request a prior authorization.
To Submit Electronically, Go To Meridianrx.com And Select “Submit Prior Authorization.”
Only 1 medication per form all fields must be completed and legible for review. Prior authorizations cannot be submitted over the phone. Web effective april 1, 2022, the electronic prior authorization (epa) form will no longer be an acceptable form of submission. If an authorization is needed, you can access our login to submit online.
Web Medication Prior Authorization Request Phone:
Web welcome michigan complete members. • full name of member • member’s date of birth • member’s meridian id number Prior authorizations should be submitted through the new provider portal or via fax. Web meridian prior (rx) authorization form.
Web Prior Authorization Is Required Before Certain Services Are Rendered To Confirm Medical Necessity As Defined By The Member’s Plan.
Please visit our new prior authorization website page to gain access to the secure portal and correct fax forms here. Primary care provider reassignment form. Web some covered services or medications may need approval from meridian, this is called a prior authorization (pa). The following information is required for meridian to accept your authorization request:
You Do Not Need A Paper Referral From Meridian To See A Provider, But Your Provider May Need To Request A Prior Authorization From.
A physician may be able to secure insurance coverage and obtain clearance to prescribe the proposed medication once the below form has been. Weight watchers® exhausted benefit form Mobile crisis response provider reference guide.